Did you know that you can die from opiate withdrawal?
We didn’t.
When we first started this project in November 2017, we had little knowledge of opioids beyond the basic understanding that they were responsible for the current public health crisis. As political scientists, we wanted to know how opioids affect local communities and what government was doing about it.
To date, we have conducted more than one hundred interviews with doctors, nurses, social workers, lawyers, peer advocates, activists, people in recovery, and more. We’ve listened to people talk about the challenges rural communities face — like limited transportation and fewer treatment options — and how people navigate their way around them — for example, by leveraging the criminal justice system to get loved ones into treatment.
We’ve learned a lot just by talking to people in their communities, but, like us, many people still have questions about what kinds of treatment are the most effective and where to go for help. “What is the cutting-edge research showing?” one person asked. In this blog, we consult both the research and the law to debunk five myths about opioid-related treatment in New York State.
Myth #1:
You can’t die from opiate withdrawal.
When people dependent on opioids go to the hospital for detox, they’re often turned away on the grounds that withdrawal won’t kill them. “There’s no real danger coming off of heroin,” one hospital social worker explained. However, “[w]hen it’s alcohol and benzos … chances are we are probably going to admit.”
When people suddenly decrease or stop consuming either alcohol or benzodiazepines — psychiatric medications commonly prescribed to treat anxiety and depression — they are at risk for experiencing life-threatening seizures and delirium tremens. For this reason, patients dependent on these substances are typically admitted to the hospital for detoxification, whereas people dependent on opioids, who often experience severe flu-like symptoms, are not. This tendency to underestimate the dangers of opiate withdrawal and turn people away results from the common misperception that “no one dies” from it.
Failure to monitor and treat the symptoms of opiate withdrawal can (and does) result in death.
Contrary to popular wisdom, death from acute opiate withdrawal is uncommon but not unprecedented. Withdrawal symptoms may include nausea, fever, sweating, vomiting, diarrhea, and hypertension, among others. If left untreated, persistent vomiting and diarrhea can result in heart failure caused by hypernatraemia (elevated blood sodium levels) as well as severe dehydration. Patients with comorbid conditions, such as coronary artery disease, congestive heart failure, HIV, or liver failure, are also at increased risk of death. Aside from the physical complications of opiate withdrawal, the desperate actions people take to relieve their symptoms (such as buying more illicit opioids) are also life threatening. Failure to monitor and treat the symptoms of opiate withdrawal can (and does) result in death.
Myth #2:
Hospitals can’t provide detoxification services because they don’t have a detox unit.
Given the risks associated with opioid withdrawal, hospitals play a key role in saving lives. Oftentimes people present at emergency departments either seeking detoxification by their own free will or, more commonly, following an overdose reversal with Narcan. Between 2016 and 2017, emergency room visits for opioid overdoses increased by nearly 30 percent. A psychiatrist at one hospital estimates that they see two to three overdoses a day, some even in the parking lot. But, like most hospitals, they don’t have a certified detoxification unit. Instead, when people wake up from an overdose in the emergency department, most of them just leave. “[W]e encourage, we educate, we support,” explained one hospital social worker. “But once they say they want to leave they can leave. There’s no regulatory standard that says you have to be held here against your will.”
Under New York State Mental Hygiene Law, a certificate is required for hospitals to operate a detoxification unit. A “unit” is defined as “the provision of chemical dependence withdrawal and stabilization services in excess of 5 beds, or greater than 10 percent of overall patient days.” Consequently, hospitals are reluctant to admit patients for detoxification services unless they hold the requisite certificate, otherwise they risk reimbursement.
Under the existing waiver, every medical/surgical bed in a hospital can be used to provide detoxification services, and hospitals can receive reimbursement for them.
Because the refusal to admit for detox is “a missed opportunity that could potentially have fatal consequences,” the New York State Office of Alcoholism and Substance Abuse Services (OASAS) issued a time-limited waiver in March 2018 authorizing hospitals to run more than five detox beds without first obtaining a certificate. The only stipulation is that hospitals are asked to send an email to OASAS notifying it of their intent to expand detoxification services. Under the existing waiver, every medical/surgical bed in a hospital can be used to provide detoxification services, and hospitals can receive reimbursement for them. The waiver, which was initially set to expire on December 31, 2018, was recently extended to December 31, 2019. However, only six hospitals have contacted OASAS regarding their intent to take advantage of this opportunity. They are:
> Cortland Regional Medical Center (Cortland)
> Flushing Hospital Medical Center (Queens)
> UPMC Chautauqua at WCA (Jamestown)
> Joseph’s Medical Center (Yonkers)
> Jamaica Hospital Medical Center (Queens)
> Auburn Community Hospital (Auburn)
Myth #3:
Peer engagement services cannot be billed to Medicaid.
Expanding detoxification services is one part of the overall effort to improve access to addiction treatment in New York State. Increasing peer-support services is another. A comprehensive review of the research found that peer recovery support can lead to “reduced relapse rates, increased treatment retention, improved relationships with treatment providers and social supports, and increased satisfaction with the overall treatment experience.” However, a common misconception among drug treatment providers and hospitals is that they cannot bill for these services.
Part of the confusion stems from the fact that different types of peer workers exist: e.g., certified addiction recovery coaches (CARC), peer-engagement specialists, and sponsors. Yet, only the services provided by certified recovery peer advocates (CRPA) are reimbursable under Medicaid. A certified recovery peer advocate is someone who is in recovery themselves, or has a close family member in recovery. CRPAs help people with substance-use disorders navigate the obstacles of getting into treatment and support people when they return home. Under existing regulations, CRPAs must be supervised by a credentialed or licensed clinical staff member. However, confusion about whether and how much to bill for peer-support services can deter providers from utilizing them.
| Requirements | Certified Recovery Peer Advocate | Certified Addiction Recovery Coach |
| Certification Board | New York Certification Board | New York Certification Board |
| Training | 46 hours of training Recovery Advocacy : 10 hours Mentoring & Recovery: 10 hours Recovery & Wellness: 10 hours Ethics for Peer Professionals: 16 hours | 60 hours of training Recovery from Addiction: 20 hours Recovery Coaching: 20 Hours Recovery Education: 5 hours Ethical Responsibility: 15 hours |
| Examination | Required | Not required |
| Other | 500 Hour Work Requirement 500 hours of work experience as a volunteer, CRPA provisional, or CARC, including 25 hours of supervision by a qualified supervisor | Annual Renewal Requirement 6 hours of Addiction Recovery Coaching including at least 1 hour of NYCB approved ethics |
| Reimbursable | Yes | No |
In billing for services, licensed clinicians must develop a treatment plan that includes the clinical reasons for peer-support services, establish goals for treatment, and identify next steps. For their part, peer advocates must provide a note for each visit, including the duration and overall purpose of the service. The format for billing and reimbursement is a fee-for-service model. For additional information on how to become a CRPA or bill for services, see this guidance document and toolkit published by OASAS.
It’s worth noting that while financial considerations weigh heavily on the minds of providers, still other concerns exist. Some agencies, for example, worry about liability and whether a signed consent form is necessary for peer advocates to be in the room. Still others don’t fully understand what CRPAs do. “Many of the staff are confused about the role of CRPAs,” one training director explained. “They need to know that the CRPAs are there for very specific duties and that they shouldn’t be used to do anything clinical. They shouldn’t be sent to go get coffee and lunch for the staff [or] … to do all of the filing. They have a very specific duty and the staff need to be educated just like the CRPAs need to be educated.”
Myth #4:
MAT is substituting one drug for another.
Beyond detoxification and peer-support services, hospitals can administer medication-assisted treatment (MAT). MAT is nothing new in the United States. Pilot studies testing methadone maintenance for heroin addiction, for example, began in 1964, followed by formal Food and Drug Administration (FDA) approval in 1972. When used properly, methadone reduces cravings for opioids without causing euphoria, suppresses the symptoms of withdrawal, and blocks the effects of heroin.
The FDA has since approved two additional medications for preventing opioid relapse including buprenorphine (e.g., Suboxone which is taken daily in pill form) and naltrexone (e.g., Vivitrol which requires a monthly shot). Buprenorphine is a “partial opioid agonist,” which means that it mimics “full agonists” (such as oxycodone, fentanyl, and heroin) by attaching to opioid receptors in the brain. However, it does so imperfectly. Partial attachment eases withdrawal symptoms and reduces drug cravings without causing the same euphoric effect as full agonists (see this helpful guide for patients from the Women’s College Hospital). Typically, doctors will start patients on Suboxone during the early stages of withdrawal in order to minimize the painful symptoms that can lead to relapse.
Naltrexone, by comparison, is an “opioid antagonist,” which means that it blocks opioid receptors in the brain and prevents people from feeling the effects of taking opioids. Unlike Suboxone, people who take extended-release antagonists like Vivitrol must complete detoxification first. A new study comparing buprenorphine to naltrexone found that, because naltrexone requires going through full withdrawal, people have a substantially more difficult time getting started on the medication. However, once over the “induction hurdle,” naltrexone and buprenorphine exhibit similar effects. For example, results indicate that the opioid relapse rate for naltrexone was approximately 52 percent, compared to 56 percent for buprenorphine. These findings are consistent with other studies and extensive literature reviews showing that MAT significantly reduces the chances of opioid-related relapse and even death.
Despite the known benefits of MAT, its use is controversial. Perhaps the most common objection is that medication-assisted treatment amounts to little more than the substitution of one drug (methadone, buprenorphine, or naltrexone) for another (oxycodone, hydrocodone, heroin, and fentanyl). Thus, opponents argue that the goal of treatment should not be to put people on medication but instead to abstain from all substances. “The thinking that created the problem shouldn’t solve the problem,” said one women in recovery at a New York Summit. “Yet people are pushing for solutions run by the pharmaceutical companies.”
In contrast to the abstinence-only approach, proponents of medication-assisted treatment argue that it is necessary to save lives. “We are not treating a drug with a drug,” explained one addiction specialist. “We are treating a substance-use disorder with a medication.”
Amid growing acceptance of the disease model of addiction, supporters often liken MAT to other prescribed medications (such as taking insulin for diabetes). However, the potential for diversion and misuse is real. Studies show that people can misuse buprenorphine by injecting or snorting the crushed tablets, while others sell it on the street to make a profit. Thus, the most effective MAT programs typically combine medication-assisted treatment with intensive drug-monitoring activities, therapeutic counseling, and vocational resources and referrals.
While it is unlikely that the treatment community will reach a consensus on MAT anytime soon, the road to recovery is long and varied. Perhaps the best we can do, then, is to respect people’s decisions about what kinds of treatment work best for them. “It’s your recovery,” one counselor explained. “You are the one who drives the train.”
Myth #5:
High-quality treatment is out-of-state treatment.
Over the past year, we’ve spoken to several parents who sent their children out of state for addiction treatment, or at least considered the option. Oftentimes, these decisions were rooted in the perception that long-term treatment is inaccessible or that local facilities offer substandard care. Throughout the course of our interviews, overreliance on outpatient care (often caused by insurance restrictions), outdated treatment facilities, inferior halfway housing, and the lack of wraparound services were all cited as powerful disincentives to seek addiction treatment locally.
By comparison, the alleged benefits of traveling out of state are enticing: people can seek treatment anonymously; remove themselves from known triggers in their environment; or pursue special treatment options that aren’t available locally, e.g., flotation tank therapy. The fact that some of the most widely advertised facilities are “nestled in the hills of Malibu, California” or the beautiful southwest deserts of Arizona doesn’t hurt either. Oceanfront property, serene desert landscapes, and plush backyards dotted with barbeque grills appeal to most people, suffering from addiction or not.
While luxury residences and tranquil getaways sound and look appealing, treatment fraud is a real issue.
While luxury residences and tranquil getaways sound and look appealing, treatment fraud is a real issue. No doubt, credible rehabs exist outside New York State. However, others are exploitative. For example, unscrupulous providers will pay “lead generators” $50 dollars for a single referral, with the understanding that they can reap $40,000 or more in insurance claims. The now infamous “man-in-blue” ad, featuring a bearded young man in blue scrubs wearing a stethoscope (pictured in the photo illustration at the top of this post), is emblematic of the deceptive marketing techniques used to lure patients. Sponsored by the Addiction Network, a twenty-four-hour call center based in Southern California, the ad promises free consultation and referral services. However, the agency does not verify whether a provider is reputable. Instead, callers are “automatically routed to a rotating list of treatment centers, which prepay to receive a set number of calls per month.”
The so-called “Florida model” has come under attack due to its not-so-obvious shortcomings. While luxury rehabs do an excellent job getting people in the door (paying for expensive advertising, promising cutting-edge treatment, and offering free one-way plane tickets), “they don’t have the natural connections … to the community services that are essential for continued recovery.” As one provider put it, for-profit entities “take people out of their communities, bill insurance, run the insurance dry,” and then turn people out without first connecting them to aftercare services at home.
Despite the difficulties people can have accessing treatment, New York State has one of the largest drug treatment systems in the United States. In 2016, there were 279,744 admissions to New York State substance use treatment programs. By comparison, the next two largest state programs admitted 152,548 (California) and 95,414 (Maryland) people, respectively. When asked why so many New Yorkers continue seeking treatment elsewhere, one residential provider explained that it was because local nonprofits lack the resources needed to compete on the market for drug treatment, even though they offer more comprehensive care; e.g., residential treatment followed by outpatient treatment in or close to people’s community of origin. “It’s one of the best kept secrets in New York State,” he explained, “that there is treatment available.”
Conclusion
At a time when many people to turn the internet for answers to questions about drug treatment, separating fact from fiction is crucial to informed decision making and action. Indeed, the simple fact that people can and do die from opioid withdrawal should prompt more hospitals to reexamine their admission criteria and take advantage of the time-limited waiver to expand detoxification services. Getting informed, learning about different treatment options, and understanding the rules and regulations that govern access to care are necessary steps in dispelling the myths that prevent people from getting the treatment they deserve.
ABOUT THE AUTHORS
Katie Zuber is the assistant director for policy and research at the Rockefeller Institute of Government
Patricia Strach is the director for policy and research at the Rockefeller Institute of Government
Elizabeth Pérez-Chiqués is a visiting fellow at the Rockefeller Institute of Government
SUGGESTED CITATION
Katie Zuber et al., “Five Myths of the Opioid Crisis,” Rockefeller Institute of Government, February 7, 2019, https://rockinst.org/blog/five-myths-of-the-opioid-crisis/.
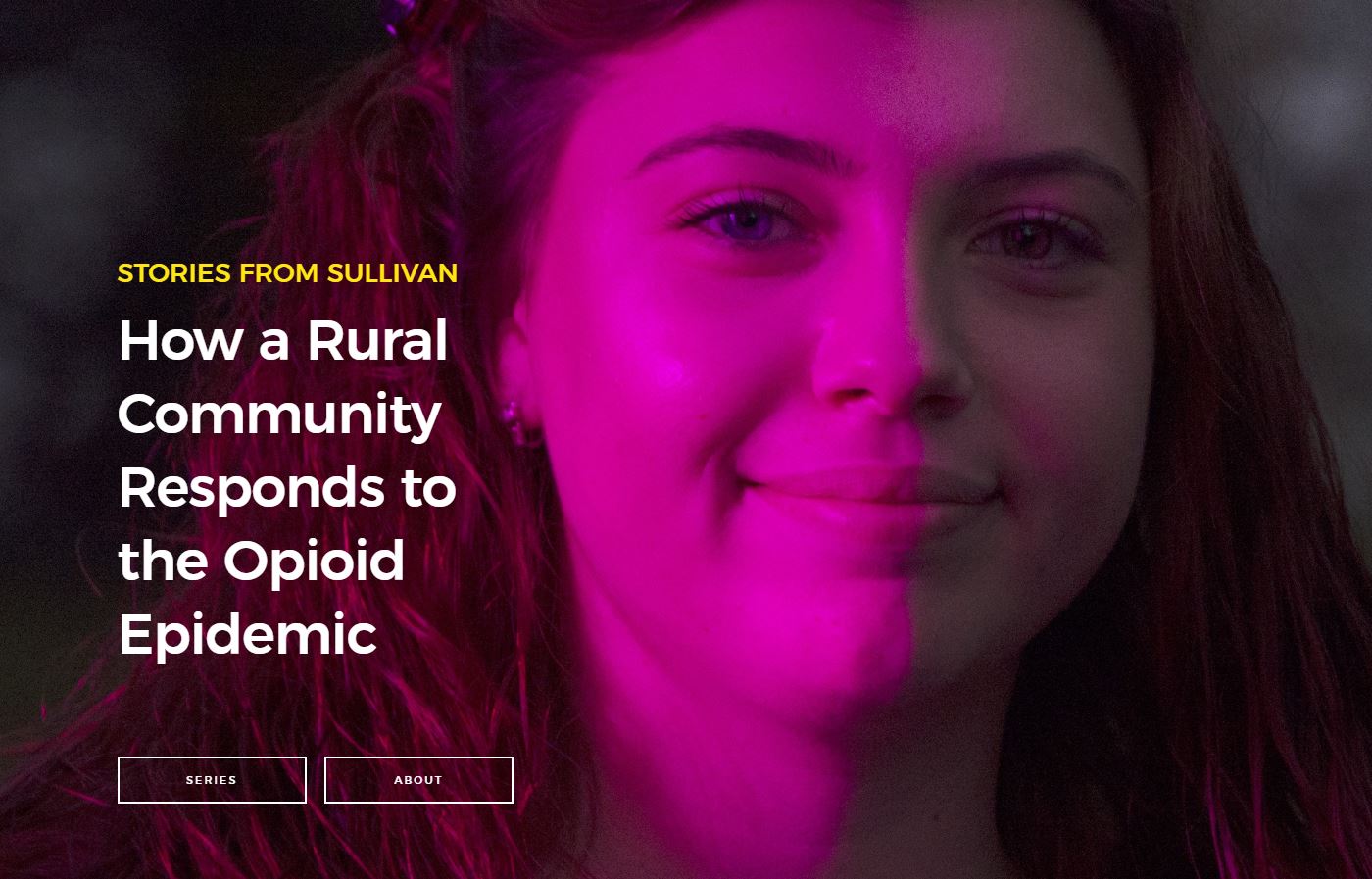
READ THE SERIES
The Rockefeller Institute’s Stories from Sullivan series combines aggregate data analysis with on-the-ground research in affected communities to provide insight into what the opioid problem looks like, how communities respond, and what kinds of policies have the best chances of making a difference. Follow along here and on social media with the hashtag #StoriesfromSullivan.